Come As You Are

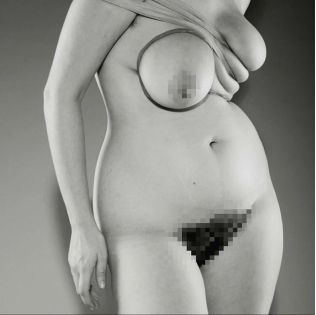
It’s time to re-meet your maker, with Par Femme's modern guide to vaginal wellness
A recent survey of outpatients at a UK teaching hospital found that only nine per cent of respondents could correctly label female genital anatomical structures on a diagram; nearly half left that section blank. Research continues to show that even someone with a vagina of their very own may be unable to navigate its physical topography, let alone understand its complex inner workings. But it’s unsurprising, given what history shows us.
In ancient Greece, Hippocrates (widely known today as the ‘Father of Medicine’) popularised the idea of the ‘wandering womb’, wherein medical afflictions identified in women were explained as the result of the neglected uterus having dislodgied itself from the pelvic region and ‘wandering’ aimlessly around the body. In 1857, British physician Edward Tilt asserted that travelling by train, riding horses or even listening to music while menstruating could aggravate women’s ovaries. As late as the 1960s in the United States, non-consensual clitoridectomies were performed as ‘treatment’ for hysteria, erotomania and lesbianism.
In 2021, the Australia Talks National Survey found that more than one in three women said they’d had health concerns dismissed by a GP. History has been rough on the female body, and while barriers to education and threats to bodily autonomy persist today—especially for people who aren’t wealthy, white, cisgender men—attitudes are shifting. By building an understanding of the female anatomy’s physiology, delicate ecology and relationship to pleasure, we can pursue a closer connection with this long- maligned part of the body and, in turn, a more intimate relationship with ourselves.
We consult three of Australia’s leading vaginal health innovators about the importance of pelvic health, vaginal microbiome and the next wave of pleasure products addressing pain and anxiety in sex.
Pelvis: Strength Training
Ask someone who has given birth and they may tell you just how much of an impact pelvic health can have on a person’s body and wellbeing. Ruth Schubert, a pelvic floor physiotherapist and founder of Exhale Physiotherapy in Byron Bay defines pelvic health as wellness in the region from belly button to mid-thigh. Schubert assists patients experiencing difficulties with bladder, bowel, gynaecological and sexual function, treating weakness disorders (stress urinary incontinence, faecal incontinence, pelvic organ prolapse, reduced sexual sensation) and overactivity disorders (overactive bladder, bladder pain syndrome, obstructed defecation, anorectal pain and sexual pain).
Women are likely to experience at least one of several issues that can lead them to seek guidance from a pelvic physiotherapist, according to Schubert, and age isn’t always linked to the concern. But, thanks to thousands of years of learned embarrassment and misdiagnosis, women aren’t always willing to ask for help. ‘Often women with pelvic health dysfunction suffer in silence, because they feel like they are the only one with these conditions,’ Schubert explains. ‘But we know that these are relatively common concerns with a whole host of evidence-based treatment options to help.’
"Like any form of wellness, prevention is better than cure."
Schubert explains that pelvic health issues often span beyond the immediate area. ‘For example, pelvic floor dysfunction can significantly impact a woman’s ability to exercise. For one in two women, urinary incontinence negatively impacts exercise participation, and pelvic organ prolapse affects exercise for 28 per cent of women, which means a whole host of women are missing out on the health benefits of exercise.’
According to Schubert, women experiencing prolapse and incontinence have a higher risk of poor body image and decreased sexual health, and urinary incontinence in older women has even been associated with decreased socialisation and increased risk of depression, sometimes leading to earlier admission into nursing home care. ‘Like any form of wellness, prevention is better than cure. Working out a plan and maintaining consistency with your exercises can prevent pelvic floor dysfunction in the future,’ Schubert says. For weakness disorders, this means strengthening the pelvic floor with daily exercise. The pelvic floor—a group of muscles and ligaments whose primary role is to support the pelvic organs—is commonly associated with childbirth, but it’s also part of the core muscles that are important to overall wellness. A strong pelvic floor adds to sexual function, helps to prevent prolapse, and stops bladder and bowel leaks. Schubert says that strengthening the pelvic floor muscle is usually the first line of treatment for weakness disorders, and can be very effective for many women.
‘The pelvic floor muscles comprise deep and superficial layers, with the deep muscles attaching from the pubic bone to the tailbone in a sling-like shape about three centimetres above the level of entrance of your vagina,’ she says. ‘We can strengthen our pelvic floor by doing voluntary contractions of the muscles to fatigue. The contraction should be as if you are holding in wind, holding in urine and lifting up towards your head. At the end of the contraction you should relax the muscle back to its starting position.’ The use of kegel balls or other types of vaginal weights can also be beneficial. Overactivity disorders can be managed by working with a pelvic physiotherapist to reduce the sensitivity, tenderness or tightness in the pelvic floor region, and adopting good bladder and bowel habits can reduce straining and pain.


pH: An Intimate Ecology
Much has been said about the microbiome over the past decade, about the community of micro-organisms living together on the skin or in the gut. As it turns out, the vaginal microbiome deserves some attention as well. According to Moira Bradfield, a naturopath, acupuncturist and the founder of Gold Coast-based holistic health service Intimate Ecology, the vaginal microbiome acts kind of like a bouncer, blocking any microbes that want to waltz on in and disturb your vagina’s carefully cultivated environment, usually through the pathways of sex, hygiene or menstruation.
‘The vaginal microbiome shares some common characteristics with the skin and gut microbiome, such as protection against invading pathogens, production of essential nutrients and compounds,’ Bradfield says. One of the key ways the vaginal microbiome differs from the gut microbiome, she continues, is its diversity. ‘Sites like the gut are considered healthy when they have a lot of different types of microbes, whereas the vagina is considered to be more balanced when there are high amounts of Lactobacilli bacteria. Generally, these bacteria contribute to the acidity of the vagina—the pH level—which also helps in controlling balance.’
Maintaining the equilibrium of the vagina’s pH is how experts can assess the health of a vagina. When the environment is destabilised, conditions can occur as a result of bacterial or fungal imbalances. Bradfield names bacterial vaginosis (BV) as the most common, characterised by a reduction in Lactobacilli and an increase in a number of different microbes. These other microbes, known as anaerobic microbes, are the culprits when it comes to a milky-looking discharge or fishy aroma.
Another common cause for treatment is vulvovaginal candidiasis (VVC) or, as you’ll no doubt know it, vaginal thrush. Most women have felt the infuriating prickle of thrush at some stage, which can often be triggered by a course of antibiotics or contraceptives that contain estrogen. ‘Thrush usually presents with a classic cottage cheese discharge, inflammation, itch and swelling, and can be caused by a number of different Candida species with the most common being Candida albicans,’ Bradfield explains.
‘Taking care of overall microbiome health in all sites can also help your vaginal health, with a balanced diet, regular relaxation and self-care.’
The good news? Imbalances such as BV or VVC are relatively simple to solve. ‘Both of these conditions can occur as one-off infections but for many can recur and are experienced on a regular basis,’ explains Bradfield, who notes that the known cause isn’t always obvious. ‘The vaginal ecology is also influenced by hormonal fluctuations, and lifestyle and sexual interactions, and sexually transmitted infections (STIs) don’t always have symptoms, which is why getting tested is so important.’
Most concerns can be treated by over-the-counter medications, particularly if they aren’t causing problems on a regular basis and you’re only in need of short-term relief. But if it’s recurring, Bradfield suggests further investigation to pinpoint any underlying issues, such as hormones, lifestyle factors, and pH disruptors, which could be exacerbating the infection. ‘Not everything is thrush, and not everything is microbial. There are also dermatological, immune and allergic issues that can impact the delicate tissues of the vagina and vulva,’ she says. ‘If you have concerns that aren’t easily addressed or that recur, measure your vaginal pH, track symptoms to the day in your cycle, monitor your diet, sexual interactions and stress. This can reveal patterns in your hormones or lifestyle that may be impacting the microbiome or could be easily modified to provide relief.’
This may sound complicated, but there are a number of easy steps that can help maintain vaginal health. Take a regular vaginal health prebiotic, consider your underwear choice (Bradfield advises that synthetic fabrics can cause issues for some people) and examine the ingredients, materials or cleanliness of anything you’re allowing near it, from lubricants, which should be pH-appropriate, to sex toys, period care and even your partner’s personal hygiene. ‘We’re talking about an important microbial space that needs to be considered in relation to what you put in it and on it,’ says Bradfield.
‘Taking care of overall microbiome health in all sites can also help your vaginal health, with a balanced diet, regular relaxation and self-care.’ A little discharge can also be an indicator of a healthy hormonal pattern and fertility. ‘A change in discharge is generally something to investigate with your health care professional if it’s accompanied by other symptoms, which might be evidence of a microbial shift,’ Bradfield says. ‘You will have different amounts of discharge at different life stages, so one person’s normal is different to the next. A healthcare professional can also assist in supporting overall health and identifying issues.’

Pleasure: Higher Desire
This naturally occurring chemical has become the darling of the beauty and wellness world, famed for its ability to reduce feelings of anxiety and stress. Now, cannabidiol—known more commonly as CBD—is poised to revolutionise intimate pleasure as well, particularly for people who deal with sexual pain or struggle to reach orgasm.
While CBD has become increasingly accessible in the US in recent years, its availability is lagging elsewhere, especially in Australia. As of February 2021, however, low-dose CBD products were reclassified by the Australian government from a schedule four drug, which require a doctor’s prescription, to a schedule three drug, which pharmacies can sell over-the-counter without a prescription. It’s good news for people hoping to try CBD as a way to support their health, but it may be a while for products to be widely available: at the time of publication there are no TGA-approved products on the Australian Register of Therapeutic Goods, and it can take years to get approval.
Until then, medical doctors with knowledge about the potential therapeutic benefits of CBD are the best first point of contact. One company with an CBD-based intimate product offering is Lovers, co-founded by gynaecologist and fertility specialist Dr Raelia Lew. ‘The cannabis plant has been used for medical reasons since ancient times to treat conditions such as pain and epilepsy,’ Lew explains. ‘Our goal is to assist relaxation and intensify female orgasm. We know from many descriptive studies that female cannabis users report enhanced sexual function, increased desire and greater intensity of orgasm, so by using CBD in our Easy Love formula we are helping people enjoy the benefits safely.’
It is a shocking figure that fewer than 50 per cent of women regularly experience an orgasm during sex. I want to help change that.’
While Easy Love can be used recreationally for heightened sexual pleasure, Lew emphasises its ‘life-changing’ potential for people who experience sexual concerns such as anorgasmia (inability to reach orgasm), vaginismus (involuntary tensing of the vagina), endometriosis and sexual pain. Recognising that female sexual pleasure is rarely given focus within a largely patriarchal medical culture, Lew was inspired to create products that help women address issues that were ruining their sex lives or putting them off sex altogether. ‘I also felt that there was a big gap in the market for all women seeking to enhance experiences of sex generally, with the aid of a beautiful product that was on par with the high-end skincare that they would be happy to use on their face.’
The results of personal pleasure go far beyond the confines of climax. A fulfilling sex life can also boost our physical, emotional and mental wellbeing, which can be just as important for optimal vaginal health. ‘The benefits of orgasm also extend to mental health as well as physical wellbeing, self esteem, satisfying sexual relationships, the aerobic benefits of sex, of course, and general life satisfaction,’ Lew explains. ‘It’s about all women feeling comfortable, confident and sexy,’ she says of the made-to-order brand. ‘Many women have preconceptions of what sex is to them, and I invite women to challenge that. We have myriad erogenous zones, and pleasure for us is also intimately psychosexual. It is a shocking figure that fewer than 50 per cent of women regularly experience an orgasm during sex. I want to help change that.’